Background and Significance:
The rare nature and diagnostic difficulty associated with myelodysplastic/myeloproliferative neoplasms (MDS/MPN) has limited the inclusion of patients (pts) with these diseases, other than chronic myelomonocytic leukemia (CMML), in relevant clinical trials. This has resulted in the complete lack of approved agents for the treatment of pts with non-CMML MDS/MPN. Moreover, ASTX727 (oral decitabine-cedazuridine) was approved for CMML based on a study of only 16 pts with CMML. A larger study of CMML and non-CMML MDS/MPN is needed.
MDS/MPNs appear to be BCL2-dependent (Bogenberger et al., 2015; Jilg et al., 2016), but data for venetoclax combination therapy are derived from retrospective analyses of relapsed/refractory disease (Cortes et al. 2019; Hammond et al., 2020) or single-arm studies not dedicated to MDS/MPN (NCT04655755, Venugopal et al. 2021). Venetoclax exposures are not affected by coadministration of ASTX727 and predict responses similar to historical data (Mannis et al. 2021). Based on these promising early data and the critical need, we proposed a randomized study of ASTX727 alone or in combination with venetoclax for pts with MDS/MPN and >5% blasts.
Study Design and Methods:
This is a National Cancer Institute-sponsored, multi-center, international, randomized phase 2 study (NCT05600894, NCI 10538) designed to evaluate the efficacy of ASTX727 alone or in combination with venetoclax in pts with newly diagnosed MDS/MPN with >5% marrow blasts. Key eligibility criteria include allowing hydroxyurea cytoreduction to a WBC <10,000/mm 3 for proliferative disease and excluding pts with need for emergent disease-directed therapy as well as prior therapy for myeloid malignancy other than hydroxyurea or thrombopoietic/erythropoietin stimulating agents.
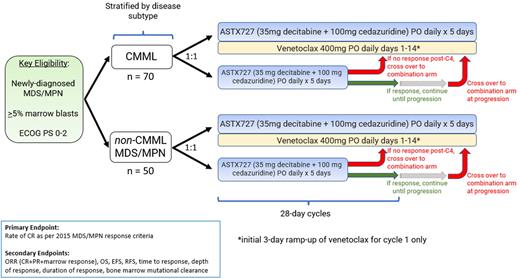
Pts will be randomized 1:1 to receive either ASTX727 alone (Days 1-5) or in combination with venetoclax, initially administered with a 3-day dosing ramp-up and given for 14 days per 28-day cycle (Figure 1). Pts are stratified by disease subtype, specifically CMML and non-CMML MDS/MPN. The primary endpoint is the rate of complete remission (adapted from the MDS/MPN-specific response criteria developed by Savona et al. 2015). Secondary endpoints include the overall response rate, overall survival, progression-free survival, allogeneic hematopoietic stem cell transplantation rate, clonality at time of hematologic remission, number of red cell and platelet transfusions required and toxicity of ASTX727 versus ASTX727 + venetoclax. Pts randomized to the ASTX727 monotherapy arm and without response after 4 cycles of therapy, or with progressive disease after an initial response, cross over to the ASTX727 + venetoclax arm. A futility analysis is planned for each cohort (first 18 and 13 pts in each treatment arm for the CMML and non-CMML cohorts, respectively).
We assume that 85% and 90% of pts in the CMML and non-CMML MDS/MPN cohorts, respectively, randomized to the ASTX727 monotherapy arm will not achieve the primary endpoint and will cross over to the ASTX727 + venetoclax combination arm. The estimated accrual time of a total of 70 pts with CMML and 50 pts with non-CMML MDS/MPN will require about 2.9 and 2.1 years, respectively.
Planned integrated studies include the use of an apoptosis multiplex immunoassay to evaluate how the addition of a BCL-2 inhibitor will influence the ability of ASTX727 to induce apoptosis and if particular thresholds of apoptosis are predictive of clinical response. Planned exploratory studies include the use of: 1) RNA-seq to evaluate if differences in baseline transcriptional programs appear to be predictive of response to ASTX727 and ASTX727+venetoclax, 2) next generation (Oncomine Comprehensive Assay (OCAv3)/whole exome sequencing to uncover biomarkers predictive of response/outcome, validate risk modeling to stratify these pts and detect/monitor measurable residual disease (MRD) on serial marrow samples that can predict depth of response with translation in improvement in event-based endpoints, and 3) circulating tumor DNA as a non-invasive means (i.e., without need for a marrow evaluation) of prospective MRD detection for prognostic use.
This ongoing, randomized study may inform frontline therapeutic options, provide prospective data for venetoclax combination after HMA failure, and generate striking correlative science for pts with “high risk” MDS/MPN.
OffLabel Disclosure:
Shallis:Gilead Sciences: Consultancy; Rigel: Consultancy; Servier: Consultancy; Bristol Myers Squibb: Consultancy; Curio Science: Consultancy. Podoltsev:Cogent Biosciences: Other: IDMC Member; AI Therapeutics; Arog Pharmaceuticals; Astellas Pharma, Inc.; Astex Pharmaceuticals; Boehringer Ingelheim Pharmaceuticals, Inc.; Celgene Corporation; CTI BioPharma Corp.; Daiichi Sankyo, Inc.; Genentech, Inc.; Jazz Pharmaceuticals, Inc.; Kartos Therapeuti: Research Funding; AbbVie Inc.; Blueprint Medicines (former); Constellation Pharmaceuticals (former); CTI BioPharma Corp. (former); Incyte Corporation (former); Novartis (former); PharmaEssentia (former): Consultancy. Patnaik:Epigenetix: Research Funding; Kura: Research Funding; CTI BioPharma: Membership on an entity's Board of Directors or advisory committees; StemLine: Research Funding. Zeidan:Novartis: Consultancy, Honoraria; Daiichi Sankyo: Consultancy, Honoraria; Taiho: Consultancy, Honoraria; Mendus: Consultancy, Honoraria; Zentalis: Consultancy, Honoraria; Jazz: Consultancy, Honoraria; Chiesi: Consultancy, Honoraria; Epizyme: Consultancy, Honoraria; Notable: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Kura: Consultancy, Honoraria; Shattuck Labs: Research Funding; Otsuka: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Orum: Consultancy, Honoraria; Lox Oncology: Consultancy, Honoraria; Geron: Consultancy, Honoraria; Regeneron: Consultancy, Honoraria; Genentech: Consultancy, Honoraria; Syndax: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Boehringer-Ingelheim: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Servier: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Syros: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Ionis: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Schrödinger: Consultancy, Honoraria; BeyondSpring: Consultancy, Honoraria; Astex: Research Funding; Tyme: Consultancy, Honoraria; Agios: Consultancy, Honoraria; Celgene/BMS: Consultancy, Honoraria; ALX Oncology: Consultancy, Honoraria; BioCryst: Consultancy, Honoraria; Foran: Consultancy, Research Funding; Amgen: Consultancy, Honoraria.
ASTX727 (decitabine/cedazuridine, approved for CMML) and venetoclax, both being used for remission induction for myeloid malignancies (CMML and non-CMML MDS/MPN)

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal